Expectations are that semiconductor industry revenue growth will accelerate to annualized double-digit levels this decade, spurred by demand for AI chips. This would be a growth rate well above levels that we’ve seen since the mid-1990s, with predictions that the roughly US$50 billion dollars of AI chips sold in 2023 could rise to US$400 billion dollars of sales before the end of the decade.

Out of
Our Minds

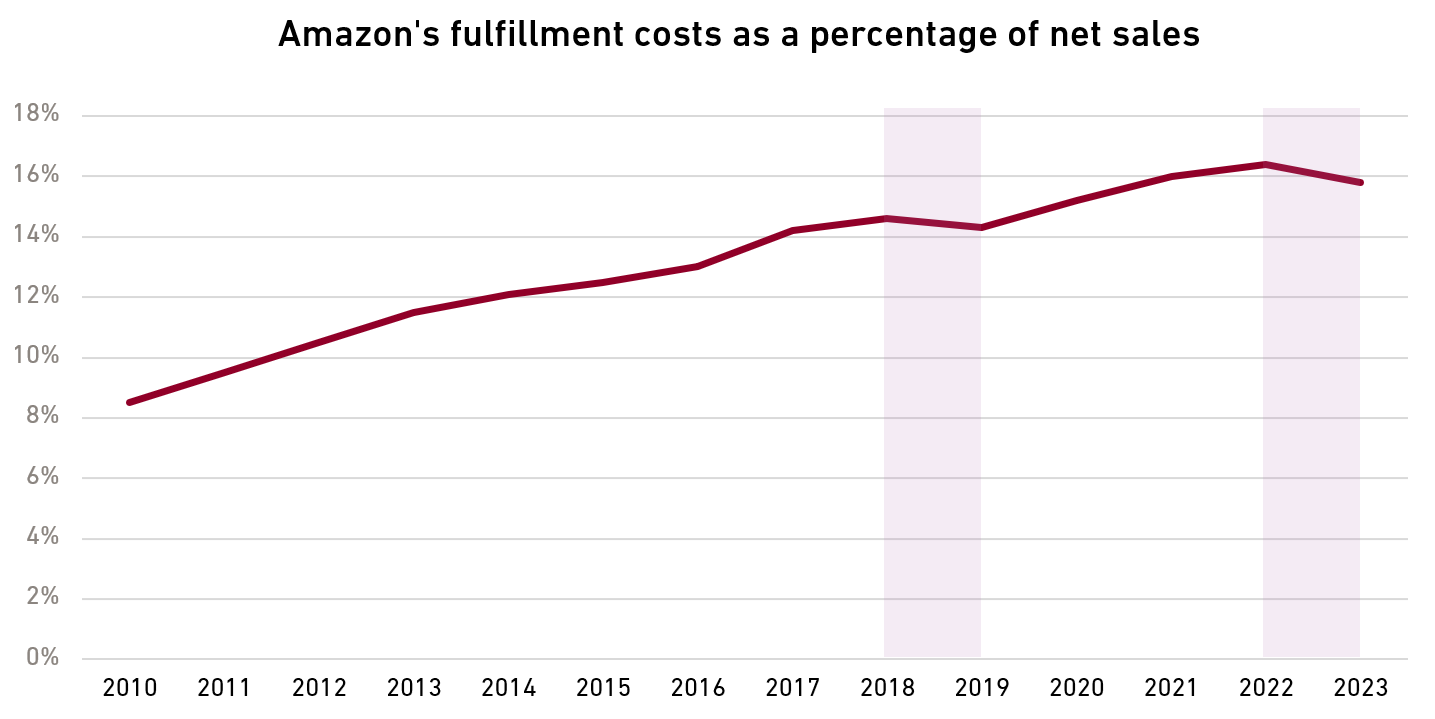
Amazon’s Latest Logistical Feat Delivers Long-Term Profit Gains
But with so much focus on AI, what is perhaps under-appreciated is that Amazon’s e-commerce business recently underwent a transformation of its own—a rethinking of how it gets customers’ packages from point A to point B. Because of this new strategy, the business, where profitability has been low and erratic, may be on the cusp of a new era in which margins finally reach—and sustain—an attractive level.

Baidu Abandons Moonshots to Search for Earthly Profits

Ramadan’s Shifting Dates Have Complex Effects on Businesses
The holy month of Ramadan affects companies and products differently each year, and it is essential for investors in Muslim-majority countries to understand these effects. The holiday, during which Muslims fast from dawn to dusk, starts 10-12 days earlier each year, unlike fixed holidays such as Christmas. This year, Ramadan starts at sunset on March 10 and lasts until April 9.
Ramadan’s Slowly Shifting Seasonality
Timing of Ramadan relative to Northern Hemisphere seasons, 2010-2040
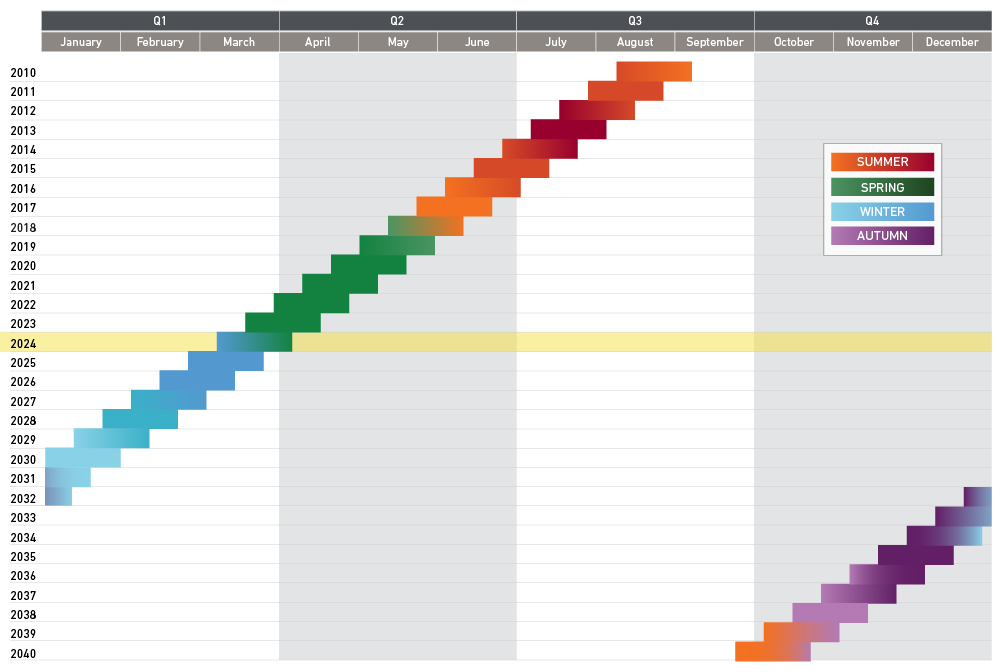
The fact that the holy month moves each year means that the effects of Ramadan on businesses change over time. Recently, when Ramadan was during the summer, it was a significant headwind for companies such as brewers, as the fast suppressed demand for beer during what would otherwise be a peak month. But now as Ramadan is moving earlier in the year, that headwind will lessen.
What did you think of this piece?

Fewer Babies Means Better Business for Diaper Maker
Japan has been undergoing a baby bust for decades. In the early 1970s, there were years where more than 2 million babies were born in Japan, but since then, those numbers have declined steadily. By the 1990s, there were about 1.2 million babies born each year in Japan, while in 2022, births fell below 800,000 for the first time.
Source: The Statistics Bureau of Japan

Can a Raw Deal Be Good for Netflix?

Japan Digging Out of Chronic Deflation One IT Worker at a Time
Analyzing Industry Structure through Porter’s Five Forces Model
As bottom-up investors, we aim to invest in high-quality growth businesses at reasonable prices to provide superior risk-adjusted returns over the long term. To determine what constitutes a high-quality growth business, we research a company’s management, financial strength, growth prospects, and we closely examine the industry in which it operates to determine the company’s competitive advantage.
It’s as important to examine a company’s industry as it is to examine the fundamentals of a company. An analysis of industry structure can inform how well-positioned a company is relative to competitors, as well as the profit potential for the company.
Our analysis is guided by Harvard University professor Michael Porter’s Five Forces, which were first introduced in a 1979 issue of Harvard Business Review and later detailed in his 1980 book, Competitive Strategy: Techniques for Analyzing Industries and Competitors.
In this six-part video series, we examine each Porter Force and discuss how we use them to analyze industries. Watch the series introduction below and click through to see how we leverage Michael Porter’s Five Forces framework for industry analysis.
What did you think of this piece?
Japan’s Past Hints at China’s Future
China faces a demographic shift similar to Japan three decades ago. Portfolio manager Jingyi Li explains how that comparison can help guide investors looking at China today.
What did you think of this piece?

NVIDIA and the Cautionary Tale of Cisco Systems
Competitive Advantage and Pricing Power
Portfolio manager Jingyi Li discusses how several Global Equities portfolio companies are using their pricing power to navigate through this period of higher interest rates and higher inflation.
What did you think of this piece?

The Democratic Republic of The Congo Could Be the Next Big Frontier Market, Eventually
Navigating Conflict in the Middle East
Portfolio manager Anix Vyas, CFA, discusses how the current conflict in the Middle East is affecting International Small Companies portfolio holding CyberArk.
What did you think of this piece?
Chinese Companies Look Better than China’s Economy
In 2023, Chinese markets have been roiled by continued trade tensions, slowing economic growth, and deleveraging in the property sector. Despite this difficult backdrop, there are reasons to be optimistic about the growth prospects of some Chinese companies. Portfolio Managers Andrew West, CFA, and Lee Gao discuss their current perspectives on China with Portfolio Specialist Apurva Schwartz, including how they weigh the opportunities and risks of investing in the market.
Slowdown in Economic Growth
Real estate, the biggest source of wealth for Chinese consumers, was in bubble territory and has been slowing for a while. This has negatively affected consumer confidence and household consumption.

Cable Strikes Back
I see it differently. Viewed through the lens of Michael Porter’s competitive forces, which we use at Harding Loevner to analyze industry dynamics, the dispute was a clear example of a change in the bargaining power of buyers amid the changing economics of streaming services.

Ozempic and the Substitution Trade
The twist is that Ozempic, a trade name for semaglutide, is a diabetes drug, not an obesity drug. Semaglutide is however effective in inducing weight loss; its creator Novo Nordisk markets a separate version called Wegovy specifically for obesity. Wegovy became so popular there were shortages of it, so doctors began prescribing Ozempic “off label” for a condition other than its intended use. That popularity fueled Novo Nordisk shares and this month it pushed past LVMH as Europe’s most valuable company.
Growth Opportunities from Electrification
Portfolio manager Scott Crawshaw highlights several companies in our Emerging Markets portfolio that are poised to benefit from increasing electrical power demand.
What did you think of this piece?

Meta Accelerates Its AI Game
In its second-quarter earnings conference call, Meta founder and CEO Mark Zuckerberg detailed how AI permeates the company. For example, nearly all of Meta’s advertisers now use at least one AI-based product, allowing them, for instance, to personalize and customize ads. He also touted an increase of 7% in time spent on Facebook after launching AI-recommended content from accounts that users don’t follow.
Now the company plans an aggressive push of its own version of generative AI, the kinds of large language models that have gotten so much attention lately. In July, the company released an open-source—i.e., free for even commercial use—generative AI platform called Llama 2, which Meta hopes will emerge as a competitor to OpenAI’s GPT-4. Meta is betting its platform will unleash users’ creative potential and result in a flood of content. If that occurs, Meta’s powerful algorithms for matching content with users—4 billion of them across all of its platforms—will become indispensable as a content-discovery tool with a rich set of monetization options from advertising to ecommerce to subscriptions.

Generative AI Through a Fundamental-Research Lens
Anyone who has interacted with popular AI models—asked them about the mysteries of life and the cosmos or created convincing Van Gogh replicas using AI-enabled image generators—can sense that we may be in the midst of a technological revolution. That prospect has consumed equity markets lately, with seven US tech-related stocks responsible for most of the market appreciation in the second quarter.
As an investor in high-quality, growing businesses, we have always tried to position this portfolio to benefit from secular trends, the kind that transcend economic cycles and are driven by fundamental changes in key areas such as tech. Still, it is incredibly difficult for anyone to predict how such trends will unfold; the vicissitudes of cryptocurrency are a sobering reminder of this. Furthermore, as seen with the rise of the internet and, later, mobile connectivity, technology is merely a platform; it’s the applications of the technology that eventually determine many of the winners and losers. In the case of generative AI, some of the future applications may not yet be conceivable, although many companies, even outside the tech field, are now pondering the possibilities.
India: Four Takeaways from Our Travels
Vietnam’s Labor Costs, Taxes Attract Chinese Manufacturers
Portfolio Manager Wenting Shen, CFA, and Portfolio Specialist Apurva Schwartz discuss why Chinese companies are relocating production facilities to Southeast Asia. Watch the rest of their conversation.
What did you think of this piece?

What P&G’s Pricing Decisions Tell Us About Inflation
As the world’s largest consumer-goods company, Procter & Gamble provides insight into what’s driving the pricing decisions at big brands.
How Are Earnings of Emerging Markets Companies Holding Up?
Portfolio manager Pradipta Chakrabortty discusses the earnings bright spots within emerging markets regions and sectors.
What did you think of this piece?

Small Caps: Adventures in Fundamental Research
The superheroes of the stock market—mainly US corporations valued at or close to a trillion dollars—tend to dominate investment news and research. And yet little-known small companies—often based outside the US—that never generate a headline remain some of the most vibrant sources of innovation. If the biggest large caps sell the finished products that investors and consumers know well, small caps often occupy a small niche along the global supply chain, providing a critical piece of technology known only to its intended audience.
Macro Do’s and Don’ts
One of our more acid-tongued colleagues likes to observe that “just because we don’t do macro, it doesn’t mean the macro cannot do us.” The observation is a challenge to our bottom-up investment philosophy and merits a response. What does his comment really mean? Is he correct?

Going Home: An Account from China’s “Zero-COVID” Frontline
But days before Shen’s departure, new complications arose: outbreaks of the Omicron variant in several Chinese cities, including Shanghai, were prompting citywide lockdowns. The flight was still due to depart, but had been rerouted to Fuzhou, a coastal city across the strait from Taiwan, 450 miles to the Southwest.
The natural—some would say, prudent—decision at this point might have been to postpone her trip. But Shen, worried she might not easily get another ticket, pressed ahead. Here are her travel bulletins.

A Ground’s Eye View on Inflation and Its Persistence
The outsized demand for durable goods has run headlong into the diminished supply. While the springboard for price increases may have been reduced supply, the strength and persistence of those increases, which are now feeding through to labor markets, are raising the specter that aggregate demand is outpacing even normalized aggregate supply. There is precious little that monetary policy can do to counter supply-led inflation, but—Omicron willing—it is likely to be temporary. But if inflation comes to be led by stubborn excess demand, then tight monetary policy is the orthodox response, and we can expect central banks to hit the economy over the head with a brick to prevent a sustained wage-price spiral. Demand-led inflation would have significant implications for asset prices.
Inflation is notoriously difficult to forecast; even some at the US Federal Reserve (Fed) concede that it has no working model for inflation.1 We could do no better and accordingly make no effort to forecast future inflation. What we can do is talk to the companies we own or follow and tease out the impact on their earnings from the rising input costs they’re experiencing; their changing bargaining power vis à vis their suppliers; whether they are able to pass on higher costs to their customers before stifling demand; and how all that is coloring their business outlook. The following represents what our research analysts have been able to glean from those conversations.

What’s Driving China’s Regulatory Transformation
One can only speculate on the reasons for this synchronous timing, but one possibility that stands out is the confluence of the five-year policy and leadership cycles in China. This is the first year of the 2021-25 Five-Year Plan, but more importantly, it is the final full year before the top 200 or so members of the Central Committee of the Communist Party of China are selected at its National Congress in October 2022. It bears remembering that those politicians are similar to counterparts elsewhere in facing challenges that have diverted them from other priorities. They spent the first two years of their terms coping with escalating US-China trade tensions, and just when “normal order” loomed after the signing of the Phase One trade agreement, COVID-19 hijacked everyone’s lives. Only recently have they gotten a chance to work on much-delayed goals.

Big Health vs. Big Tech: A Fight over the Future of US Health Care
Too Much Information
Indeed, when I started my career in investing in the late 1970s, obtaining even basic financial info about a German car company still required going to Germany and knocking on the company’s door.
Now gathering information no longer takes much effort. We are deluged by floods of data—not only the details of prices, volumes, margins, and capital investments of individual companies, but also highly granular data about credit card receipts, numbers of cars in parking lots, or words used in media reports. These new, “alternative” sources of information have briefly given some stock pickers a slight edge in predicting short-term stock price movements. The informational advantage provided by such data is but fleeting, however; once this data is commercially accessible to everyone, the advantage disappears. Thus, even for the short-term investor, information gathering itself no longer provides a lasting edge.
For long-term investors, the relationship to information has changed even more fundamentally. You no longer need to seek information; it finds you. Your job, rather, is to act as what Lou Gerstner, the former CEO of IBM, called an “intelligent filter”—determining the information that is important and ignoring data that (in the case of the investor) doesn’t help you forecast cash flows and estimate the value of a security.

When Will Life Return to Normal?
If we are honest with ourselves, it is a question that almost all of us, as investors and people, are probably wondering right about now. In this case, it took the form of the following note from a young colleague based in locked-down London directed to me and my fellow Health Care analyst as part of the daily, ongoing Research Information Group email discussion that has always comprised much of our meeting, brainstorm, and “water-cooler” time here at Harding Loevner.
Considering the challenges of [vaccine] manufacturing and distribution, what would be your best estimate for when developed economies will return to “normality”? I.e., people in developed economies are allowed—and feel safe enough—to live a life more like 2019. E.g., Sept 2021? Jan 2022? Never?

Out of Our Minds—From the Beginning
Disclosures
“Out of Our Minds” presents the individual viewpoints of members of Harding Loevner on a range of investment topics. For more detailed information regarding particular investment strategies, please visit our website, www.hardingloevner.com. Any views expressed by employees of Harding Loevner are solely their own.
Any discussion of specific securities is not a recommendation to purchase or sell a particular security. Non-performance based criteria have been used to select the securities discussed. It should not be assumed that investment in the securities discussed has been or will be profitable. To request a complete list of holdings for the past year, please contact Harding Loevner.
There is no guarantee that any investment strategy will meet its objective. Past performance does not guarantee future results.
© 2024 Harding Loevner